Health Policy Affairs
The Government Shutdown will not delay WISeR
On Oct 22, 2025, Abe Sutton, Director of the Center for Medicare and Medicaid Innovation (CMMI) and Deputy Administrator of the Centers for Medicare & Medicaid Services (CMS), spoke at the American Medical Association's webinar titled CMMI answers your questions on the Wasteful and Inappropriate Service Reduction (WISeR) model. In the question-and-answer portion of the webinar, he said the government shutdown will not affect the launch. Models are being developed and tested out of the Innovation Center with separate funding that Congress has already appropriated. The statutory mandate requires the innovation center to continue to test payment models.
The WISeR Model is a six-year, voluntary initiative from the CMS Innovation Center that will run from January 1, 2026, through December 31, 2031, in New Jersey, Ohio, Oklahoma, Texas, Arizona, and Washington. The program is designed to test a more efficient, transparent, and clinically sound approach to prior authorization for the selected Medicare services and policies below.
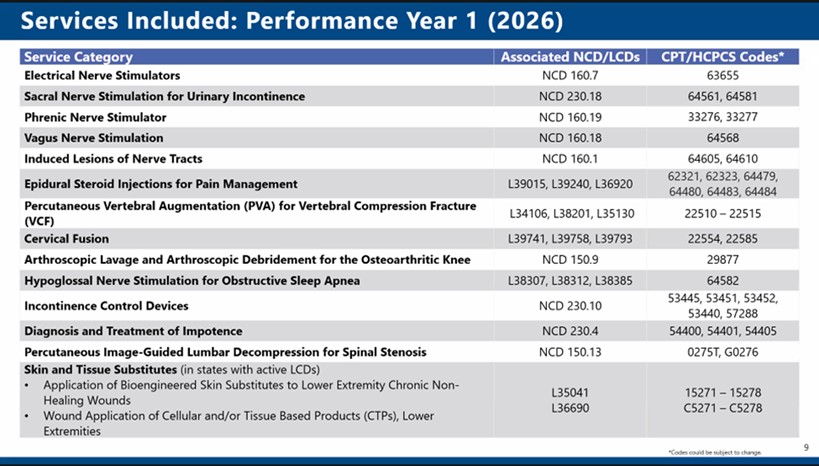
WISeR seeks to reduce administrative complexity and friction between physicians and payers by focusing on clear coverage criteria, streamlined processes, and accurate, timely determinations. Significantly, the model does not change Medicare coverage policies, payment rates, or existing appeal rights. Instead, it enforces a subset of existing National and Local Coverage Determinations (NCDs and LCDs) and emphasizes faster, more consistent decision-making.
Physicians
Physicians' participation in the selected states is voluntary. Physicians may either submit a prior authorization request or choose to bypass prior authorization and undergo a prepayment review. If a prior authorization is affirmed, the physician will include a unique tracking number with the claim. If not affirmed, the physician will receive an explanation and may resubmit the request, pursue peer-to-peer review, or appeal the decision. Physicians who bypass prior authorization will have their claims reviewed prior to payment, with full appeal rights retained in both pathways.
Gold Card program
A Gold Card program will recognize physicians who consistently meet Medicare coverage criteria, exempting them from prior authorization and prepayment review. The Gold Card Program is expected to begin in mid-2026 and will be reassessed periodically to maintain compliance standards.
The model will leverage technology and automation to improve the speed and consistency of prior authorization while requiring all medical determinations to be reviewed by a physician with relevant clinical expertise. CMS will monitor accuracy, timeliness, and physician experience throughout the model’s duration. Services included in WISER were selected based on existing coverage criteria, non-emergent status, sufficient service volume, and potential vulnerability to fraud, waste, or abuse. CMS has already removed deep-brain stimulation from the model after feedback from the physician community. The service list may be updated as evidence evolves, and CMS will notify participating physicians of any changes. The success of WISeR will be measured through metrics such as determination, accuracy, and timeliness, appeal rates, and physician and beneficiary experience. CMS will evaluate the model’s impact on care quality, administrative burden, and patient outcomes, and publish aggregate results. Ultimately, WISeR aims to model a better, less burdensome prior authorization process that aligns payment and coverage decisions with clinical evidence, physician input, and patient needs, while maintaining transparency, accountability, and access to appropriate care.
For more information, see the CMS WISeR provider and supplier guide.